What You Need to Know
Living with an autoimmune condition can feel like navigating a minefield of symptoms, flare-ups, and dietary restrictions. If you’re among the millions dealing with conditions like rheumatoid arthritis, lupus, multiple sclerosis, or Hashimoto’s thyroiditis, you’ve likely explored various dietary approaches to manage your symptoms. The ketogenic diet has emerged as a promising option for many people with autoimmune disorders, but understanding how it works and whether it’s right for you requires careful consideration.
Understanding the Connection Between Keto and Inflammation
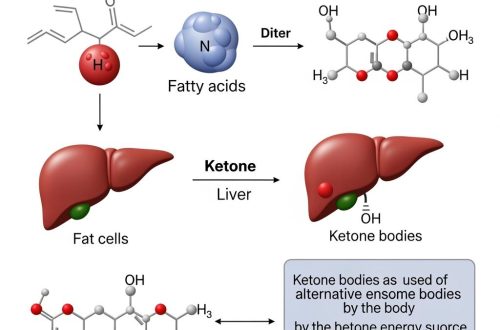
At its core, the ketogenic diet is a high-fat, moderate-protein, very low-carbohydrate eating plan that shifts your body’s primary fuel source from glucose to ketones. This metabolic shift does more than just promote weight loss – it fundamentally changes how your body produces and manages inflammation.
When you enter ketosis, your body produces beta-hydroxybutyrate (BHB), a ketone body that acts as more than just fuel. Research has shown that BHB has direct anti-inflammatory properties, inhibiting the NLRP3 inflammasome, a key driver of inflammation in many autoimmune conditions. This mechanism helps explain why many people with autoimmune disorders report significant symptom improvement on a ketogenic diet.
The reduction in blood sugar spikes and improved insulin sensitivity that come with keto also play crucial roles. Chronic high blood sugar and insulin resistance are known to fuel systemic inflammation, creating an environment where autoimmune conditions can thrive. By stabilizing blood sugar and improving metabolic health, the ketogenic diet may help calm an overactive immune system.
How Keto May Benefit Specific Autoimmune Conditions
Different autoimmune conditions may respond to the ketogenic diet in various ways. People with multiple sclerosis (MS) have reported improvements in fatigue, mental clarity, and even mobility. The neuroprotective effects of ketones may be particularly beneficial for MS, as they can provide an alternative fuel source for damaged neurons and potentially support myelin repair.
For those with rheumatoid arthritis, the anti-inflammatory effects of ketosis can lead to reduced joint pain and swelling. Many individuals report needing less pain medication and experiencing longer periods between flare-ups. The diet’s potential to promote weight loss also reduces stress on joints, providing additional relief.
Hashimoto’s thyroiditis patients often struggle with weight management and fatigue. The ketogenic diet can address both issues while potentially reducing thyroid antibodies. However, it’s crucial to work with a healthcare provider, as thyroid medication may need adjustment as symptoms improve.
Inflammatory bowel conditions like Crohn’s disease and ulcerative colitis may also benefit from keto’s anti-inflammatory effects. The reduction in fermentable carbohydrates can decrease gut inflammation and improve digestive symptoms for some individuals.

Implementing Keto Safely with Autoimmune Conditions
Starting a ketogenic diet when you have an autoimmune condition requires more careful planning than for someone without these health challenges. Your immune system is already in a delicate balance, and dramatic dietary changes can initially cause stress on the body.
Begin with a gradual transition rather than diving into strict keto immediately. Spend two to three weeks slowly reducing carbohydrates while increasing healthy fats. This approach minimizes the risk of triggering a flare-up due to the stress of rapid dietary change. Focus on anti-inflammatory fats like olive oil, avocado oil, and omega-3 rich fish rather than relying heavily on saturated fats from dairy and red meat.
Quality matters even more when you have an autoimmune condition. Choose organic vegetables when possible, grass-fed meats, and wild-caught fish to minimize exposure to pesticides and hormones that could trigger inflammation. Many people with autoimmune conditions find they do better on a “clean keto” approach that emphasizes whole foods over processed keto products.
Consider combining keto with an autoimmune protocol (AIP) approach initially. This means avoiding common inflammatory foods like nightshades, eggs, nuts, and dairy for the first 30-60 days, then slowly reintroducing them to identify any triggers. This combination can be restrictive but may provide faster symptom relief.
Potential Challenges and How to Address Them
The transition to ketosis can be more challenging for people with autoimmune conditions. The “keto flu” – temporary symptoms like fatigue, headaches, and irritability – may be more pronounced or could trigger a mild flare. Combat this by ensuring adequate electrolyte intake, especially sodium, potassium, and magnesium. Bone broth can be particularly helpful during this transition period.
Some autoimmune conditions affect nutrient absorption, making it crucial to focus on nutrient density. Incorporate plenty of low-carb vegetables, organ meats if tolerated, and consider targeted supplementation based on your specific needs. Regular blood work can help identify and address any deficiencies.
Medication interactions are another important consideration. As inflammation decreases and symptoms improve, you may need medication adjustments. This is particularly true for thyroid medications, immunosuppressants, and diabetes medications. Never adjust medications on your own – work closely with your healthcare team throughout your keto journey.
Stress management becomes even more critical when combining keto with autoimmune management. The initial adaptation period can be stressful on the body, so prioritize sleep, gentle exercise, and stress-reduction techniques like meditation or yoga.
Monitoring Progress and Adjusting Your Approach
Tracking your progress goes beyond watching the scale. Keep a detailed symptom journal noting energy levels, pain, digestive issues, and any flare-ups. Many people find it helpful to track inflammatory markers through regular blood work, including C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Be prepared to make adjustments based on your body’s response. Some people with autoimmune conditions thrive on standard keto macros (70-75% fat, 20-25% protein, 5-10% carbs), while others need modifications. You might need slightly more protein to support tissue repair or find that you feel better with carbohydrates closer to 30-50 grams daily rather than the typical 20-30 grams.
Consider cycling in and out of ketosis if strict keto becomes too stressful on your system. Some people with autoimmune conditions do well with a cyclical approach, maintaining ketosis during the week and increasing carbohydrates slightly on weekends. This can provide metabolic flexibility while still reaping many of keto’s anti-inflammatory benefits.
Working with Healthcare Providers
Open communication with your healthcare team is essential when using keto to manage autoimmune conditions. Some providers may be skeptical about ketogenic diets, so come prepared with research and be willing to compromise. Ask for regular monitoring through blood work and be transparent about all dietary changes.
Consider working with a functional medicine practitioner or registered dietitian who has experience with both ketogenic diets and autoimmune conditions. They can help you navigate the complexities of managing both simultaneously and provide personalized guidance based on your specific condition and needs.
Long-Term Sustainability and Success
Making keto work long-term with an autoimmune condition requires flexibility and self-compassion. There may be times when strict keto isn’t appropriate, such as during severe flares or periods of high stress. Having a plan for these situations – perhaps temporarily increasing carbohydrates from anti-inflammatory sources like sweet potatoes or berries – can help you maintain progress without completely derailing your efforts.
Building a support system is crucial. Connect with others managing autoimmune conditions on keto through online communities or local support groups. Sharing experiences, recipes, and strategies can make the journey less isolating and more sustainable.
Remember that healing is not linear, especially with autoimmune conditions. Some weeks will be better than others, and progress might be slower than for someone without these health challenges. Celebrate small victories, like having more energy for daily activities or needing less pain medication, rather than focusing solely on dramatic transformations.
The ketogenic diet offers promising potential for managing autoimmune conditions, but it’s not a magic cure. It’s a tool that, when used appropriately and under proper guidance, can significantly improve quality of life for many people. By approaching keto thoughtfully, monitoring your body’s responses, and working with knowledgeable healthcare providers, you can determine whether this dietary approach is right for your unique situation and potentially find relief from challenging autoimmune symptoms.





One comment on “The Ketogenic Diet and Autoimmune Conditions”
Comments are closed.